Introduction to the New Pandemic Virus
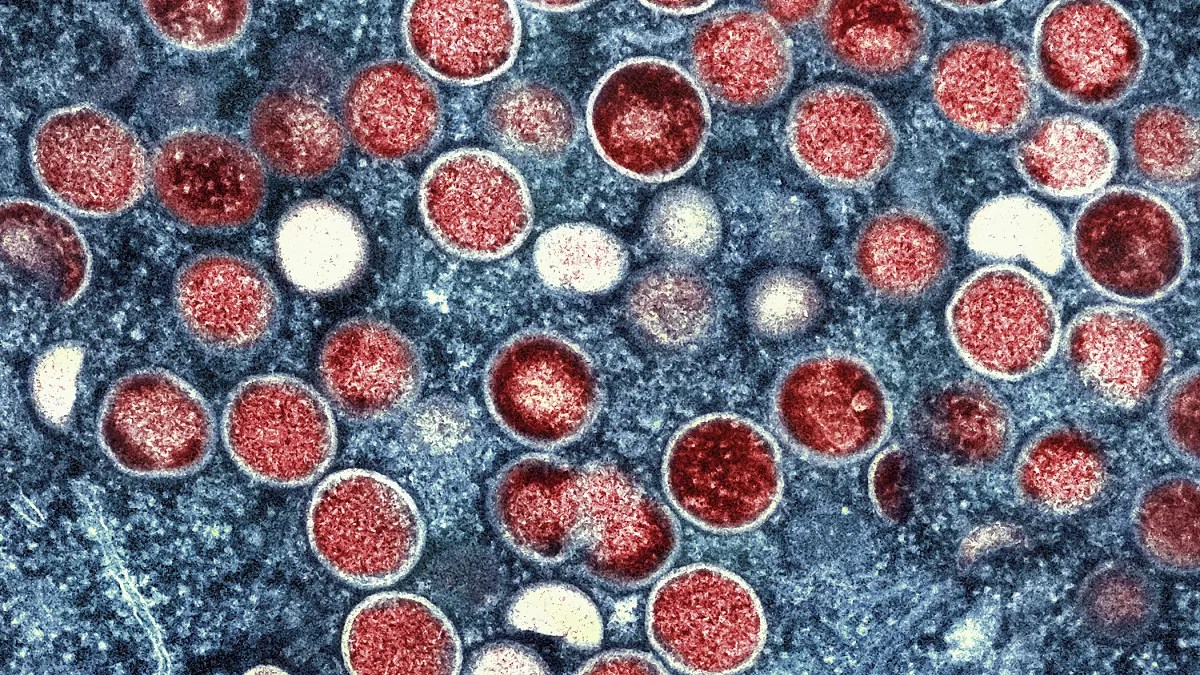
The emergence of a new pandemic virus in Africa has raised significant concerns among global health organizations and public health officials. This virus, identified in multiple regions across the continent, appears to have originated from zoonotic transmission, where the virus jumps from animals to humans. Genetic sequencing has revealed that this virus is part of a larger family of pathogens, similar in some ways to viruses that have previously led to severe outbreaks, yet it possesses unique characteristics that set it apart.
One of the primary features of this virus is its high transmission rate, which has been observed in both urban and rural areas, making containment efforts particularly challenging. Unlike previous viruses that required close contact for transmission, this new pathogen can be spread through respiratory droplets, similar to the influenza virus, emphasizing the need for heightened vigilance within communities. Initial reports indicate that the virus may present a varied symptom profile, with common manifestations ranging from mild respiratory illness to severe pneumonia, creating potential complications in diagnosis and treatment.
The implications of this new virus extend beyond Africa, as the interconnectedness of our global community fosters rapid movement of individuals across borders. Consequently, global health bodies, including the World Health Organization, are closely monitoring the situation, urging nations to enhance surveillance and implement robust preventive measures. The urgency of addressing the emerging virus is underscored not only by the potential health risks it poses within the continent but also by the likelihood of international spread, which could have far-reaching consequences. Therefore, understanding this pandemic virus’s origins and characteristics is essential in formulating effective strategies to mitigate its impact on global health.
Current Situation in Affected Regions
As of October 2023, several African countries are grappling with the emergence of a new pandemic virus, with the most affected regions demonstrating a concerning escalation in the number of reported cases and fatalities. Countries such as Nigeria, South Africa, and Kenya have emerged as significant hotspots, indicating the potential for widespread transmission. For instance, Nigeria has recorded over 15,000 confirmed cases, with a mortality rate of approximately 4%, compelling health authorities to initiate enhanced public health measures and vaccination campaigns.
In South Africa, the situation is equally alarming, with a reported incidence tenfold higher than in previous health crises. The healthcare system is experiencing unprecedented pressure, as hospitals are inundated with patients exhibiting severe symptoms. Notably, personal accounts from health care workers highlight moments of despair and the intense emotional burden they have been shouldering. Dr. Thandi Moyo, an ICU nurse from Johannesburg, remarked on the emotional toll of losing multiple patients daily, emphasizing the need for mental health support among frontline workers.
Moreover, in Kenya, health policymakers are struggling to contain the spread while addressing the critical shortage of medical supplies and personnel. The current wave of infections has severely strained the available resources, leading to significant challenges in managing patient care. Local health officials have alerted communities to practice stringent preventive measures, including social distancing and mask-wearing, to mitigate virus transmission.
In affected regions, health systems are continually adapting to the evolving landscape, with varying degrees of success. The work of healthcare professionals remains vital, as they not only treat patients but also engage in community outreach, providing education about disease prevention. Such proactive measures are essential in curbing the outbreak and protecting vulnerable populations. Health outcomes hinge not just on the availability of medical resources but also on the effectiveness of community engagement and public health messaging.
Global Health Organizations’ Response
The emergence of a new pandemic virus in Africa has prompted a swift and coordinated response from global health organizations, particularly the World Health Organization (WHO). These organizations play a critical role in monitoring outbreaks and providing essential resources and guidance to affected regions. As the new virus spread, the WHO mobilized its resources to assess the situation, gather data, and implement containment strategies aimed at curbing the virus’s transmission. This quick action is crucial for mitigating potential implications for global health.
In the early stages of the outbreak, WHO established a dedicated emergency response team to coordinate with local health authorities and assist in surveillance activities. These teams work to identify cases, conduct contact tracing, and engage in public health communication, ensuring that communities are informed about the preventive measures required to reduce transmission. The WHO also emphasizes the importance of laboratory testing to confirm cases and monitor the virus’s genetic evolution, which is vital for future vaccine development.
Resource allocation is another fundamental aspect of the response strategy employed by global health organizations. Through their collaborative efforts with international partners, WHO facilitated the distribution of medical supplies and personal protective equipment to frontline healthcare workers combating the virus. Additionally, public health recommendations were disseminated worldwide, urging countries to strengthen their healthcare systems and enhance preparedness for potential surges in cases.
The collective response also highlighted the importance of international collaboration in addressing global health threats. By engaging with various governments and non-governmental organizations, WHO has fostered an environment of shared knowledge and resources, essential for effective outbreak management. This global approach not only aids in containing the immediate crisis but also lays the groundwork for enhancing health systems and policies worldwide, preparing them for future pandemic threats.
Challenges in Containing the Virus
The emergence of a new pandemic virus in Africa presents multifaceted challenges that complicate containment efforts. One of the primary issues stems from logistical difficulties in deploying healthcare resources effectively across diverse and often remote regions. In many countries, transportation networks are underdeveloped, making it difficult to deliver medical supplies and personnel to areas most in need. These logistical hurdles are exacerbated by the vast geographic expanse of the continent, which can impede timely intervention during outbreaks.
Furthermore, the existing healthcare infrastructure in many African nations is often overstretched and underfunded. A significant lack of critical medical facilities, skilled healthcare workers, and specialized equipment diminishes the capacity to respond to a burgeoning health crisis. This deficiency is particularly notable in rural areas, where healthcare access is severely limited. In addition, many hospitals may struggle to cope with a surge in patients, leading to increased mortality rates and higher transmission of the virus among the population.
In tandem with these challenges, socio-political factors play a crucial role in the effectiveness of public health measures. Political instability, lack of governance, and ongoing conflict can hinder coordinated responses to the pandemic virus. Public trust in government institutions may be low, leading to resistance against health directives or interventions. Misinformation and the spread of false narratives regarding the virus can also undermine public health initiatives, causing individuals to ignore preventive guidelines, such as vaccination and social distancing.
Moreover, communication gaps between health authorities and local communities can contribute to confusion and fear, which ultimately impedes effective containment strategies. Inadequate outreach efforts may result in a lack of awareness and understanding of the virus, exacerbating the challenges of controlling its spread. Collectively, these factors illustrate the complexity of addressing a pandemic virus in Africa and underscore the importance of tailored strategies that account for specific regional contexts.
Vaccination and Treatment Efforts
The emergence of a new pandemic virus in Africa has prompted a swift response in terms of vaccination and treatment efforts, with multiple stakeholders collaborating to develop effective solutions. Numerous pharmaceutical companies, both local and international, have initiated partnerships to expedite the research and clinical trials necessary for vaccine approval. These collaborations have bolstered the capacity for vaccine development, resulting in promising candidates entering the trial phases, with several studies currently ongoing in various African countries. The focus on clinical efficacy and safety is paramount, as the implications of widespread vaccination will affect not only local communities but also contribute to global health security.
As trials progress, health authorities are also formulating distribution plans should these vaccines receive regulatory approval. Coordination with the Africa Centres for Disease Control and Prevention (CDC) and the World Health Organization (WHO) is critical to ensure equitable and effective distribution across the continent. Efforts are made to ensure that vaccines reach those most in need, particularly vulnerable populations who are at higher risk of severe disease. Such strategic planning is essential for maximizing the impact of vaccination campaigns when they are launched.
However, challenges remain, particularly concerning vaccine hesitancy, which poses a significant obstacle to achieving widespread immunization. Misinformation and historical distrust in healthcare systems have added layers of complexity in some African communities. This hesitancy can hinder the uptake of vaccines, ultimately affecting herd immunity and the overall success of vaccination efforts. To address this, public health campaigns aimed at educating communities about the safety and efficacy of vaccines are necessary to counteract misinformation. Building trust between healthcare providers and communities will play an integral role in the success of these initiatives, ensuring that the benefits of vaccination are fully realized.
Comparative Analysis with Past Pandemics
The emergence of new pandemic viruses in Africa invites a rigorous examination of historical precedents to identify effective strategies for response and containment. Past pandemics, such as Ebola and COVID-19, offer valuable insights into disease management and public health interventions that can inform contemporary efforts. For instance, the Ebola outbreak in West Africa from 2014 to 2016 underscored the critical importance of rapid response coordinated by local and international health organizations, highlighting the need for timely information and the mobilization of healthcare resources at a moment’s notice.
One significant lesson learned from the Ebola epidemic is the necessity of strengthening healthcare infrastructure in affected regions. The inadequacies in health systems meant that many cases went undetected initially, which allowed the virus to spread uncontrollably. By investing in health infrastructure, particularly in rural areas, current responses can be more robust, creating a framework for better surveillance and quicker interventions when a new virus emerges. Furthermore, community engagement played a pivotal role in curbing Ebola’s spread. Developing trust within communities can enhance compliance with health measures during an outbreak, an aspect that should be emphasized in recent strategies aimed at addressing the new pandemic virus in Africa.
The COVID-19 pandemic brought forth different challenges, showcasing the relevance of global connectivity and mobility. Immediate global responses such as lockdowns and travel restrictions played a vital role in limiting the virus’s spread. This aspect must also be considered as nations navigate the current outbreak. Equally important is the collaboration between governments and scientific institutions to ensure that vaccines and treatments are developed and distributed efficiently. The lessons from the challenges faced during COVID-19 regarding vaccine rollout can be instrumental in enhancing the response to emerging pandemic threats.
In summary, by understanding the experiences from past pandemics, stakeholders can adopt a more comprehensive approach, ensuring that lessons learned are integrated into current health strategies to better manage the new virus emerging in Africa and its implications for global health.
Impact on Global Health Policies
The emergence of a novel virus in Africa presents a critical juncture for global health policies, demanding immediate and comprehensive reassessment. As nations grapple with the implications of this new pandemic pathogen, it becomes imperative to enhance existing frameworks for surveillance systems. Robust surveillance is essential in detecting and identifying viral outbreaks early, allowing for timely intervention and mitigation strategies. Strengthened surveillance networks would enable countries to share vital information swiftly, thereby facilitating a coordinated response to the new virus globally.
Timely data sharing among countries plays a pivotal role in understanding the virus’s transmission dynamics, virulence, and potential spread. Transparency in reporting case numbers, outcomes, and vaccine efficacy is essential for establishing an accurate epidemiological picture. Without efficient communication, efforts to contain the virus may be hindered, potentially leading to consequences that extend beyond national borders. Thus, fostering an environment that encourages the sharing of data and best practices between nations is crucial for enhancing global preparedness against future pandemic threats.