Introduction to Cancer Treatment Innovations
The landscape of cancer treatment has undergone significant transformation in recent years, marked by continuous advancements and a multitude of innovative approaches. The rising global incidence of cancer has underscored the urgency of developing new therapies that can effectively combat this pervasive disease. According to the World Health Organization, cancer is anticipated to become the leading cause of death worldwide, further emphasizing the necessity for rapid progress in treatment modalities.
Innovative cancer treatments have emerged from rigorous scientific research, exploring areas such as immunotherapy, targeted therapy, and personalized medicine. Immunotherapy harnesses the body’s immune system to recognize and destroy malignant cells, exemplifying a paradigm shift from conventional methods that primarily relied on surgery, radiation, and chemotherapy. Targeted therapies, on the other hand, focus on specific genetic mutations within cancer cells, allowing for more precise interventions that minimize damage to healthy tissues. The rise of personalized medicine aims to tailor treatments to individual patients based on their unique genetic profiles and tumor characteristics, thereby improving efficacy and reducing adverse effects.
The integration of cutting-edge technologies, such as artificial intelligence and machine learning, has further accelerated the pace at which new treatments are being developed and refined. These technologies enable researchers to analyze vast amounts of data, identify patterns, and expedite the drug discovery process. As a consequence, a growing number of treatment options are becoming available, paving the way for future generations of cancer therapies that promise higher efficacy rates and improved quality of life for patients.
In conclusion, as we explore the latest scientific breakthroughs in cancer treatments, it is crucial to recognize the dynamic and evolving nature of this field. The imperative to revolutionize cancer therapy has never been more pressing, and continued innovation holds the key to dramatically improving patient outcomes in the fight against cancer.
Understanding the Complexity of Cancer
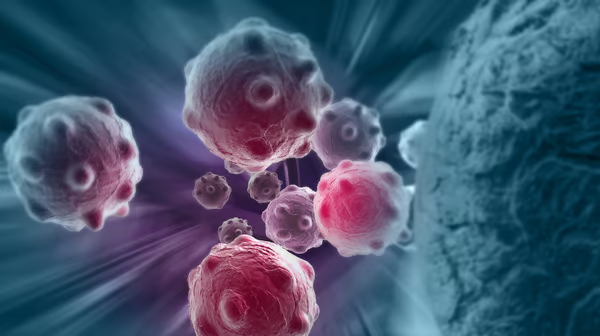
Cancer is a multifaceted group of diseases characterized by uncontrolled cell growth and proliferation. The biological intricacies of cancer begin at the cellular level, where genetic mutations disrupt the normal regulatory mechanisms governing cell cycle and apoptosis. These mutations can arise from various factors, including environmental influences, lifestyle choices, and inherited genetic predispositions. Understanding how these alterations lead to malignant transformation is crucial for developing effective treatment strategies.
As cancer cells proliferate, they can invade surrounding tissues and migrate to distant organs through a process known as metastasis. This dissemination complicates treatment efforts, as tumors can become heterogeneous in nature, exhibiting different characteristics even within the same patient. For instance, a primary tumor may respond favorably to chemotherapy while metastatic sites display resistance, highlighting the urgent need for personalized medicine in oncology.
Furthermore, the cancer microenvironment plays a vital role in tumor progression and treatment resistance. Interactions between cancer cells and surrounding stromal cells, immune cells, and extracellular matrix components contribute to a supportive niche that fosters cancer growth. This environment can protect tumor cells from the immune system and therapeutic interventions, making eradication significantly more challenging. Therefore, innovative therapeutic methods must account for these complex relationships and adapt to the dynamic nature of cancer. This includes exploring novel immunotherapies, targeted therapies, and combination treatments designed to overcome resistance mechanisms and enhance efficacy.
In essence, comprehending the biological underpinnings of cancer is fundamental for advancing treatment methodologies. As researchers unveil the depths of these complex processes, the landscape of cancer therapy continues to evolve, promising new avenues for combating this pervasive disease.
Immunotherapy: Harnessing the Body’s Immune System
Immunotherapy represents a paradigm shift in cancer treatment, leveraging the body’s immune system to identify and eliminate cancer cells. This innovative approach differs significantly from traditional treatments such as chemotherapy and radiation, which often target not only malignant cells but also healthy tissues. Recent advancements in immunotherapy have opened new avenues for more targeted and effective treatments, leading to improved patient outcomes and survival rates.
One of the most notable breakthroughs in this field is the development of immune checkpoint inhibitors. These agents work by blocking proteins that restrain the immune response against tumors, thus allowing T cells to effectively attack cancer cells. Key examples include pembrolizumab and nivolumab, which have shown success in treating melanoma, lung cancer, and other malignancies. These therapies have demonstrated the ability to induce lasting responses and even cure some patients, underscoring their transformative potential.
Additonally, CAR T-cell therapy exemplifies another cutting-edge approach within immunotherapy. This process involves engineering a patient’s T cells to express chimeric antigen receptors (CARs) that recognize specific tumor antigens. Once reintroduced into the body, these modified cells can proliferate and persist, actively targeting and destroying cancer cells. This technique has delivered remarkable results in hematological cancers, such as certain types of leukemia and lymphoma, prompting ongoing research into its application in solid tumors.
Furthermore, cancer vaccines are being developed to educate the immune system on how to distinguish cancer cells from normal cells. By introducing specific antigens associated with tumors, these vaccines aim to elicit a robust immune response. This approach is in its early stages but has shown promise in areas such as prostate cancer and melanoma.
Overall, immunotherapy has revolutionized cancer treatment, providing new hope for patients by harnessing the body’s innate defense mechanisms. With ongoing research and clinical trials focusing on enhancing its effectiveness, immunotherapy stands at the forefront of oncological advancements, driving the quest for more personalized and effective cancer treatments.
Targeted Therapies: Precision Medicine at Work
Targeted therapies represent a significant advancement in the field of oncology, transforming the approach to cancer treatment by focusing on the unique genetic and molecular characteristics of each tumor. Unlike traditional chemotherapy, which indiscriminately attacks rapidly dividing cells, targeted therapies are designed to interfere with specific pathways vital to cancer cell survival and growth. This precision medicine aims to hone in on the underlying mechanisms that foster cancer development, making treatment more effective and reducing collateral damage to healthy tissues.
The development of targeted therapies is rooted in extensive research into cancer genomics and the molecular biology of tumors. Scientists now understand that various types of cancer arise from distinct genetic alterations. For example, breast cancers that overproduce the HER2 protein can be treated with trastuzumab (Herceptin), a targeted therapy that blocks this receptor, thus diminishing the growth of HER2-positive tumors. Additionally, molecular profiling technologies allow clinicians to analyze a patient’s tumor for specific genetic mutations, which facilitates personalized treatment plans that align with the patient’s unique cancer profile.
Recent breakthroughs in targeted therapies have introduced novel agents targeting not only common mutations but also rare variants. For instance, by utilizing drugs that target specific driver mutations, such as mutations in the EGFR gene in lung cancer, more patients are experiencing improved outcomes compared to standard treatments. Moreover, advancements in immunotherapy are also interlinked with targeted therapies, as certain combinations can activate the immune system to recognize and attack cancer cells more efficiently.
The continuous evolution of targeted therapies represents a burgeoning field within oncology. As researchers unveil more about the genetic landscape of cancers, it is anticipated that these therapies will become a standard component of cancer management, paving the way for more individualized, effective treatment modalities. Such innovations underscore the promise held by precision medicine in the fight against cancer, ultimately aiming for enhanced survival rates and improved quality of life for patients.
Gene Editing: The CRISPR Revolution in Cancer Treatment
The advent of gene editing technologies, particularly CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats), has marked a significant turning point in the landscape of cancer treatment. This precise and versatile tool allows scientists to modify genes at specific locations within the genome, presenting a remarkable opportunity to rectify genetic mutations associated with cancer. The implications for cancer therapy are profound as researchers explore ways to leverage CRISPR to not only target cancer cells directly but also to develop personalized treatments tailored to an individual’s unique genetic makeup.
Recent clinical trials have showcased the potential of CRISPR in combating various forms of cancer, illustrating its ability to disrupt the function of oncogenes—genes that, when mutated, contribute to cancer development. For instance, trials focusing on hematological malignancies, such as leukemia and lymphoma, have reported promising outcomes following the application of CRISPR-based techniques to engineer T-cells. These modified T-cells, designed to specifically recognize and attack cancerous tissues, have demonstrated encouraging responses in patients, shedding light on the technology’s transformative potential.
Moreover, CRISPR’s adaptability extends to correcting genetic defects that predispose individuals to cancer. Researchers have been investigating ways to use this technology to repair mutations in genes responsible for tumor suppression, offering hope for preventive strategies in high-risk populations. The ability to not only treat but also prevent cancer through gene editing represents a paradigm shift in oncology, moving from traditional approaches to innovative, targeted therapies.
As the scientific community continues to unlock the capabilities of CRISPR in oncology, ongoing studies will be vital in determining the long-term efficacy and safety of these interventions. While challenges remain, the advances in gene editing herald a new era in cancer treatment, one that promises to improve survival rates and enhance quality of life for countless patients.
Combination Therapies: A New Approach to Treatment
In recent years, the landscape of cancer treatment has undergone significant transformation, particularly with the rise of combination therapies. This approach involves utilizing multiple treatment modalities—such as chemotherapy, immunotherapy, and targeted therapies—concurrently or sequentially to enhance therapeutic effectiveness. The rationale behind combination therapies is rooted in their potential to reduce drug resistance, a prevalent challenge in oncology. By employing varied mechanisms of action, these strategies attempt to attack cancer cells from multiple angles, significantly improving the chances of treatment success.
Recent scientific findings underscore the efficacy of combination therapies in managing various types of cancer. Research has shown that when agents with different mechanisms are combined, there is a synergistic effect that can lead to superior outcomes. For instance, in the case of melanoma, studies have demonstrated that combining immune checkpoint inhibitors with targeted therapies yields higher response rates compared to monotherapy. Such findings have prompted many oncologists to reevaluate traditional treatment protocols and consider multi-agent regimens as standard practice.
Furthermore, the use of combination therapies has been instrumental in addressing the challenge of tumor heterogeneity. Cancer cells often exhibit diverse genetic and phenotypic characteristics, which can lead to variations in treatment response. By deploying different treatment modalities, healthcare providers can better tailor therapies to individual patient profiles, improving overall effectiveness. This customization not only fosters more personalized medicine but also increases the likelihood of overcoming treatment resistance that may develop over time.
In conclusion, the adoption of combination therapies represents a pivotal shift in cancer treatment paradigms. As ongoing research continues to validate this approach, it becomes increasingly clear that utilizing multiple therapeutic avenues can significantly enhance patient outcomes and redefine the way cancer is treated. By integrating this methodology into clinical practice, oncologists move closer to achieving more effective and sustainable cancer care solutions.
Nanotechnology in Cancer Treatment: A Game Changer
Nanotechnology has emerged as a transformative approach in the quest for more effective cancer treatments. By manipulating materials at the nanoscale, scientists are able to create nanoparticles that can significantly improve the delivery and efficacy of cancer therapies. These tiny particles, typically ranging in size from 1 to 100 nanometers, hold immense potential due to their ability to interact with biological systems at a molecular level.
One of the most impactful applications of nanotechnology in oncology is in drug delivery. Traditional chemotherapy often suffers from a lack of precision, affecting both cancerous and healthy cells. However, with the employment of nanoparticles, it becomes possible to target cancer cells specifically. For instance, nanoparticles can be designed to carry chemotherapeutic agents directly to tumors, minimizing side effects while maximizing treatment effectiveness. This targeted approach not only enhances the therapy’s potency but also reduces the necessary dosage, which in turn lowers the risk of adverse reactions.
In addition to drug delivery, nanotechnology facilitates advanced imaging techniques that enable the early detection and diagnosis of cancer. Nanoparticles can be engineered to bind to cancer cells, making them more visible during imaging procedures. This enhanced imaging capability leads to earlier intervention, which is critical for improved patient outcomes.
Furthermore, the unique properties of nanoparticles allow for the development of new cancer therapies, such as hyperthermia and gene therapy. For instance, nanoparticles can be used to generate localized heat to destroy tumors without damaging surrounding healthy tissue. Similarly, by encapsulating therapeutic genes within nanoparticles, scientists can deliver them precisely to cancer cells, promoting targeted treatment strategies.
Overall, the integration of nanotechnology into cancer treatment represents a paradigm shift in oncology. With ongoing research and innovations in this field, the potential to enhance treatment effectiveness and patient quality of life continues to expand.
Challenges and Future Directions in Cancer Research
Cancer research and treatment continue to evolve, yet significant challenges prevail, impacting the pace at which advancements can be translated into clinical practice. One fundamental challenge is funding; researchers often depend on governmental and private grants to support their studies. Fluctuations in funding availability can hinder long-term research projects, especially those requiring extensive resources and time. Moreover, the allocation of funds can sometimes favor more established research avenues over innovative approaches, stifling novel ideas that may lead to breakthrough treatments.
Accessibility is another pressing issue in the field of oncology. Despite the advancements in cancer therapies, not all patients benefit equally due to disparities in healthcare access. Geographic location, socioeconomic status, and insurance coverage often dictate the level of care a patient receives. This inequity can prevent individuals from receiving cutting-edge treatments, which, in turn, impacts overall cancer survival rates. Furthermore, public awareness is critical; many patients may not be informed about novel therapies or ongoing clinical trials, which limits their treatment options and potential access to groundbreaking care.
Looking ahead, researchers aim to address these challenges through various means. For instance, there’s a growing emphasis on collaborative research efforts that pool resources across institutions, which can lead to enhanced funding and shared expertise. In terms of accessibility, telemedicine and mobile health technologies offer promising pathways to bring treatments closer to underserved populations. Additionally, increasing public awareness about new therapies and clinical trials can empower patients and encourage them to seek innovative treatment options.
By tackling funding issues, improving accessibility, and enhancing public engagement in cancer research, the translation of scientific breakthroughs into standard oncology practices can be expedited, ultimately leading to more effective cancer care for a broader population.
Conclusion: The Hope for Cancer Patients
Recent advancements in cancer treatment have ushered in a new era of hope for patients and their families. The breakthroughs discussed in this article demonstrate the remarkable progress being made in the fight against cancer. From targeted therapies that specifically attack cancer cells to innovative immunotherapies that leverage the body’s own immune system, these developments showcase a departure from traditional treatment modalities. This shift towards personalized medicine is pivotal as it offers tailored approaches that cater to the unique genetic makeup of each individual’s tumor, thus enhancing efficacy and minimizing side effects.
Furthermore, the emergence of precision oncology, which integrates genomic profiling into treatment planning, has provided a foundation for making informed therapeutic decisions. By understanding the molecular drivers of a patient’s cancer, oncologists can select the most effective treatment strategies, resulting in improved survival rates and quality of life. The promise of CAR T-cell therapy and monoclonal antibodies also illustrates significant advancements in engineering the immune response to recognize and eliminate malignant cells.
However, despite these monumental strides, the journey is far from complete. Continuous research and development are essential to uncover further innovative treatment options and address the challenges that persist in cancer care. The complexity of the disease necessitates efforts to explore new avenues, including combination therapies and novel drug delivery systems, to enhance the overall cancer treatment landscape.
In summary, the advancements in cancer treatment provide a beacon of hope. Encouragingly, as researchers and clinicians work collaboratively to push the boundaries of what is possible, the outlook for cancer patients remains positive. The commitment to ongoing investigation and understanding reinforces the shared vision of a future where cancer is managed more effectively, and patients can look forward to brighter tomorrows.